The Role of AI in Radiology
November 13, 2025
Artificial intelligence (AI) has transformed nearly every corner of healthcare, and radiology is one of the fields seeing the fastest acceleration. AI’s potential in radiology was documented early; one widely cited 2018 review concluded that “deep learning shows performance comparable to human experts in medical imaging” across multiple tasks (Rajpurkar et al., 2018). In the years since, both image-based and text-based AI tools have rapidly evolved, supporting detection, classification, quantification, and workflow optimization.
But while imaging gets most of the attention, data-oriented applications of AI in radiology are equally transformative. Much of the value in radiology lives in the text, with reports, impressions, recommendations, patient histories, and metadata scattered across the EHR. Extracting this information has traditionally required thousands of hours of manual chart review. Now, with modern LLMs, healthcare teams can use AI not only to interpret images but also to manage downstream data efficiently and safely.
In this article, we’ll explore the full radiology AI landscape, from imaging interpretation to radiology data abstraction, and show how tools like Brim make these capabilities accessible for clinical workflows, research, registries, and more.
Key Takeaways
- AI supports radiology across both imaging and text-based processes, from detection to data management.
- Image-based AI shows strong performance in detection, classification, and quantification tasks.
- Text-focused AI unlocks large amounts of data hidden in radiology reports and EHR notes.
- Purpose-built tools like Brim help teams safely deploy LLMs for structured abstraction, research, and workflow automation.
Use Cases of AI in Radiology Imaging
AI’s impact on radiology is most often discussed through the lens of image-based AI: models that analyze pixels from CT, MRI, X-ray, or ultrasound. These technologies have shown meaningful improvements in sensitivity, specificity, and workflow efficiency.
According to a 2025 comparative review, AI systems demonstrated sensitivity ranging from 63.0–98.6%, compared to 41.2–92.0% for junior radiologists, and specificity from 83.3–98.6% vs. 72.2–100% for junior radiologists when evaluating certain liver lesions (Younger et al., 2025). These results illustrate both the potential and the variability of imaging AI: promising in many contexts, but still requiring careful integration and clinical oversight.
Below are examples of how AI meaningfully contributes to core radiologic tasks.
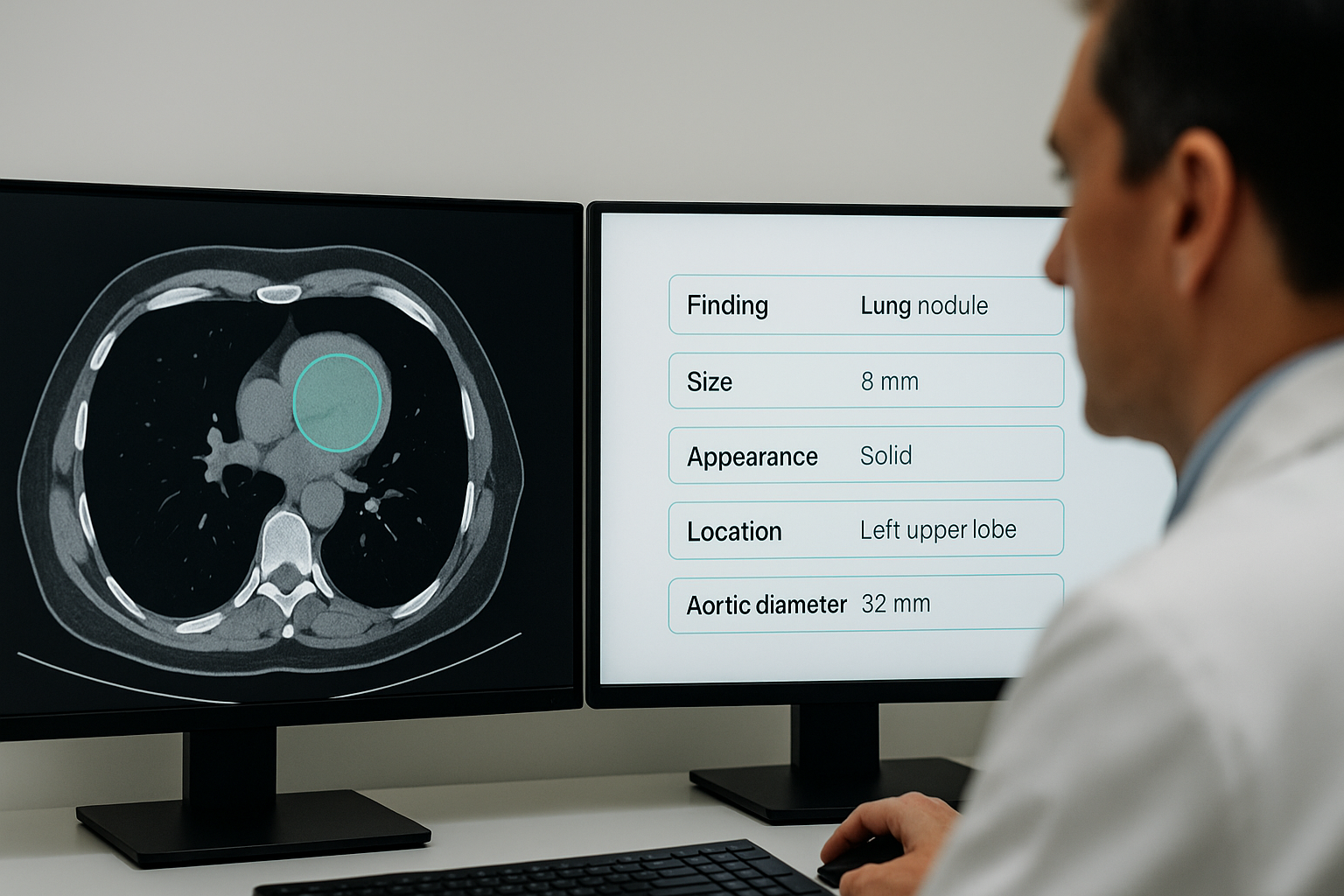
Detections
One of the most widely used applications of AI in radiology is automated detection. AI excels at identifying subtle findings that can be missed in high-volume environments. Examples include detecting lung nodules on CT scans, breast cancers on mammography or digital breast tomosynthesis, pulmonary emboli on CTPA, intracranial hemorrhages on CT, fractures on X-ray, pneumonia or COVID-related consolidations on chest X-ray, abdominal free air on CT, and deep venous thrombosis on ultrasound. By flagging these abnormalities in the background, AI can increase sensitivity, prioritize urgent findings, and support clinicians in delivering timely care.
Classification
AI also plays an important role in determining what a finding represents. Classification models analyze imaging characteristics to categorize nodules (eg solid vs. subsolid, benign vs. suspicious), assist in BI-RADS scoring for breast imaging, classify liver lesions under systems like LI-RADS, differentiate fracture types on orthopedic imaging, identify disc herniations or stenosis in spine imaging, and detect pulmonary disease patterns such as emphysema or interstitial lung disease subtypes. These models can help reduce reader variability and improve the consistency of follow-up recommendations across a radiology department or multi-site research consortium.
Quantification
Quantitative imaging is an area historically limited by the manual effort needed to measure and track findings. This has become dramatically more scalable with AI. Algorithms can measure tumor volumes to track treatment response, calculate coronary calcium scores from CT scans, generate precise measurements of aortic aneurysms, assess left ventricular ejection fraction from cardiac MRI or echocardiograms, estimate bone age in pediatric radiology, and quantify brain atrophy in neurodegenerative diseases. These tools can improve reproducibility and enable objective comparisons over time, which is especially valuable for clinical research and population health studies.
Other Imaging Use Cases
Beyond detection, classification, and quantification, AI is increasingly used to improve image quality and acquisition. For example, deep learning reconstruction techniques enable lower-dose CT scans while maintaining diagnostic quality, and MRI acceleration models shorten scan times by reconstructing high-resolution images from undersampled data. AI-driven protocol optimization helps technologists tailor acquisition parameters to patient body habitus or clinical indication automatically, reducing repeat imaging and radiation exposure. These operational improvements enhance productivity while maintaining or improving diagnostic quality.
How Can AI Help Radiology Data Management?
While imaging AI gets most of the headlines, an equally important opportunity lies in the textual side of radiology. Reports, clinical notes, prior imaging summaries, and follow-up recommendations all contain valuable information, but they are unstructured and time-consuming to extract.
A 2021 systematic review found that radiology NLP has historically been limited by model complexity, training data requirements, and generalizability challenges (Casey et al., 2021). With modern LLMs, however, these limitations are rapidly diminishing.
Here are several high-impact, text-focused use cases, many of which Brim supports directly.
Scheduling
Radiology scheduling is more complex than meets the eye. Determining which patients need rescheduling due to risk factors, contrast considerations, missed appointments, or clinical updates often requires manual review of chart notes, prior imaging, and provider communication.
In one scheduling example, a clinic using Brim previously spent 320 hours per month manually identifying high-risk patients whose surgeries needed rescheduling. By automating the initial review with Brim's LLM-based abstraction pipeline, they reduced the task to a single afternoon for a single clinician. This kind of efficiency gain illustrates how much latent value lies in clinical workflow optimization, including scheduling.
Report Generation
AI can analyze imaging notes and interpretations to produce draft radiology reports. One study generating radiology reports using ChatGPT "out of the box" found that clinicians believed the AI-generated findings to be correct 82% of the time (Bosbach et al., 2023). Clinicians also gave feedback that the ChatGPT-generated reports tended to be too verbose.
We believe that adding a structured layer to text problems like these can produce stronger results. With Brim, teams can define the exact elements desired in a radiology report, including impressions, measurements, follow-up recommendations, and structured fields, and then validate them against their dataset. Because every data element is explicitly defined and linked to evidence before being formatted in a custom way, there is greater traceability and control of the output.
Easier Participation in Research and Registries
Radiology reports hold crucial data for clinical research: response to therapy, new lesion appearance, tumor size, disease progression, and more. AI can extract this information and convert it into structured variables for downstream use in research or registry pipelines. This unlocks large volumes of data that have historically been inaccessible.
Brim’s work accelerating drug repurposing efforts demonstrates the value of quickly abstracted data in research. Values derived from radiology reports could help teams analyze treatment response at scale, and use that data downstream for registry submission or retrospective research.
Assist with Managing Follow-up
Follow-up recommendations are often buried in the impression section of radiology reports or scattered across progress notes. AI can extract these recommendations and generate structured outputs for clinicians, making it much easier to close the loop on incidental findings, routine surveillance, or high-risk cases. This improves care coordination and reduces the risk of missed follow-up.
Quality Compliance
Radiology quality programs require periodic review of imaging appointments, protocols used, adherence to standards, and documentation completeness. AI can extract relevant details from clinical notes or reports, enabling automated quality checks and streamlined audits.
Challenges of Using AI in Radiology
Although the promise is enormous, challenges remain.
A 2024 review found that generic LLMs achieved only ~50% accuracy in radiology-related tasks when used “out of the box,” without domain-specific prompts or structured workflows. We take a few conclusions from this:
Purpose-built systems are essential.
AI performance varies significantly across modalities, populations, and equipment. A system trained on one hospital’s CT scanners may not generalize well to another’s. Careful validation is essential before deploying AI clinically. Purpose-built abstraction systems like Brim enable fast and data-driven validation and customization to various environments.
A Need for Structure and Guardrails
Unstructured prompts yield unpredictable results. Radiology requires precision, so AI systems must be anchored by structured variables, data definitions, and rigorous hallucination checks. Tools like Brim provide these safeguards.
Humans must Stay in the Loop
AI is powerful, fast, and scalable, but it still makes mistakes. In order to avoid negative impact, humans need to be involved in important AI tasks, and given the context to evaluate and correct the conclusions that AI tools are making. Brim's system prioritizes showing the in-document context for every variable in order to enable this kind of collaboration.
Workflow Integration Challenges
Even strong pipelines can underperform if they do not integrate well into the radiologist’s workflow. Alerts that fire too frequently, or not frequently enough, risk disengagement. Useful AI products will need to be thoughtfully integrated into the workflow to avoid creating novel problems.
Where AI in Radiology Data is Going
Before modern LLMs, radiology NLP was constrained by available algorithms and the extensive training data required for them to perform well.
Today, foundational models are widely available, highly capable, and cost-effective. Brim uses these models because they are fast, cheap, and easy for institutions to obtain, and high performance can be achieved through fine-tuning, purpose-built tooling and validation.
Recent research shows that when AI operates on well-defined variables, accuracy rises dramatically—one study demonstrated 96% accuracy for GPT-4 on structured CT extraction tasks (Sacoransky et al., 2024).
Brim was designed to enable the future of radiology:
- Easy configuration of structured variables
- Built-in hallucination checks and constraints
- A Variable Scorecard that guides iteration to stronger variable
- A built in Validation Tool to leverage existing datasets.
- Rapid optimization workflows during review
- All in your secure environment.
These capabilities help teams harness AI for radiology safely and effectively.
Bottom Line
AI is reshaping radiology, from pixel-level detection to large-scale data abstraction. Imaging AI enhances diagnostic sensitivity and consistency, while text-based AI unlocks vast amounts of hidden clinical information. When paired with structured variable design, modern LLMs provide high accuracy and real-world reliability.
Brim helps radiology, research, and clinical teams take advantage of the advances in text-based AI without requiring machine learning expertise. With Brim, you can define, validate, and operationalize radiology workflows at scale, whether for scheduling automation, registry participation, data quality, or clinical research.
Want to learn more? Reach out for a demo.